Walking Off the Glucose: The Physiology of Insulin and Postprandial Activity
Jun 03, 2025
In an era where metabolic dysfunction is epidemic, improving insulin sensitivity should be a cornerstone of every trainer’s long-term client strategy. One of the most evidence-supported and practical tools? Walking after meals.
This article dives into the physiology of insulin signaling, glucose uptake, and why postprandial walking has such a profound effect on blood glucose control and insulin function.
Insulin: The Gatekeeper of Glucose Homeostasis
Insulin is an anabolic peptide hormone secreted by the β-cells of the pancreas in response to elevated blood glucose, primarily after carbohydrate ingestion.
Its main roles include:
-
Facilitating glucose uptake into muscle and adipose tissue via GLUT-4 translocation
-
Suppressing hepatic glucose output
-
Promoting glycogen synthesis, lipogenesis, and protein synthesis
Insulin binds to the insulin receptor (IR) on target tissues, activating the insulin receptor substrate (IRS) and downstream PI3K/Akt signaling cascade. This ultimately causes GLUT-4 transporters—stored intracellularly in muscle and adipose cells—to migrate to the plasma membrane, allowing glucose entry into the cell.
In insulin-resistant states, this signaling cascade is impaired, leading to chronic hyperglycemia and compensatory hyperinsulinemia.
Muscle Contraction vs. Insulin Signaling: Parallel Pathways
Skeletal muscle is the largest site of insulin-stimulated glucose disposal, accounting for ~70-80% of glucose uptake in the postprandial state [DeFronzo, 1988].
But what’s fascinating is that muscle contraction stimulates GLUT-4 translocation independently of insulin.
-
During movement, AMP-activated protein kinase (AMPK) and CaMK (calcium/calmodulin-dependent protein kinase) are activated.
-
These promote GLUT-4 movement to the membrane—even in insulin-resistant muscle cells [Holloszy, 2005].
This means walking post-meal offers an alternative route to glucose clearance, bypassing impaired insulin signaling in at-risk populations.
Walking Post-Meal: Evidence for Improved Insulin Sensitivity
1. Reduced Postprandial Glucose Excursions
-
Reynolds et al. (2016) found short bouts of walking (3x10 min) post-meal were more effective at reducing postprandial glucose than a single 30-minute walk [Reynolds et al., 2016].
-
Standing or walking for just 2–5 minutes every 20–30 minutes can also significantly reduce glucose and insulin responses [Dempsey et al., 2016].
2. Enhanced Insulin Sensitivity
-
Post-meal activity reduces glucose spikes, which may in turn lower chronic insulin demand, supporting improved insulin sensitivity over time [Colberg et al., 2016].
3. Improved Metabolic Flexibility
-
Regular postprandial activity supports mitochondrial adaptations, fat oxidation, and metabolic flexibility—all critical for long-term insulin responsiveness.
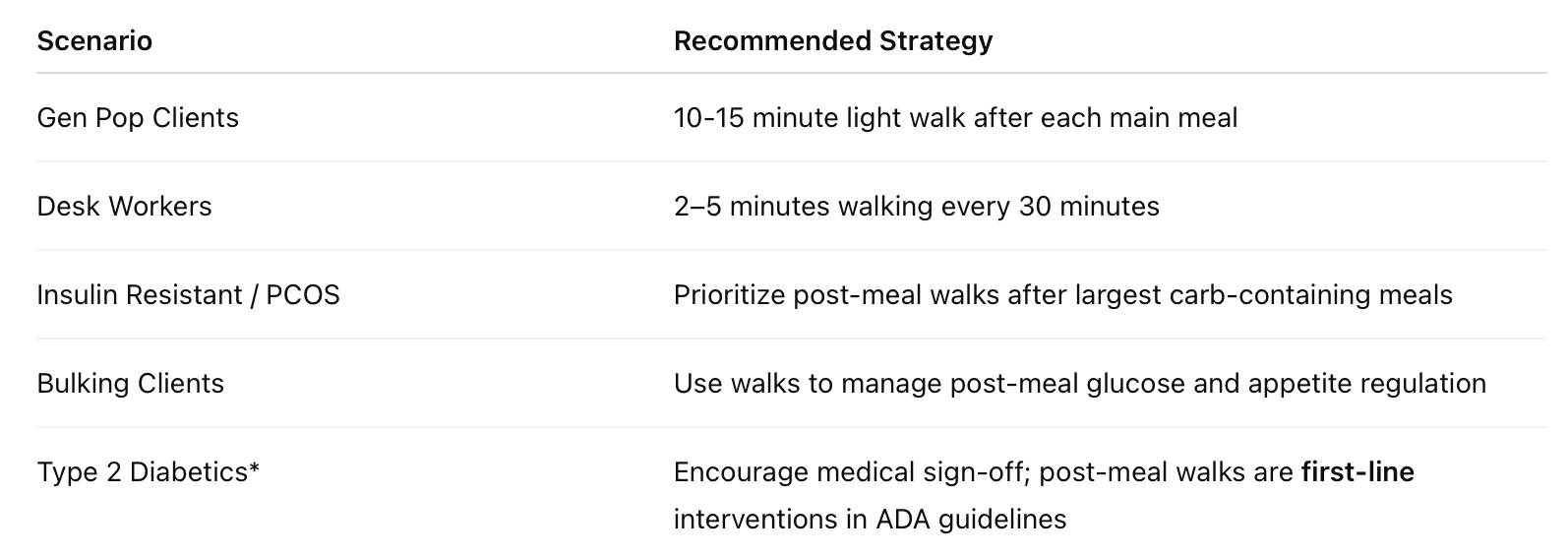
Practical Application for Coaches
Here’s how trainers can implement and coach this concept:
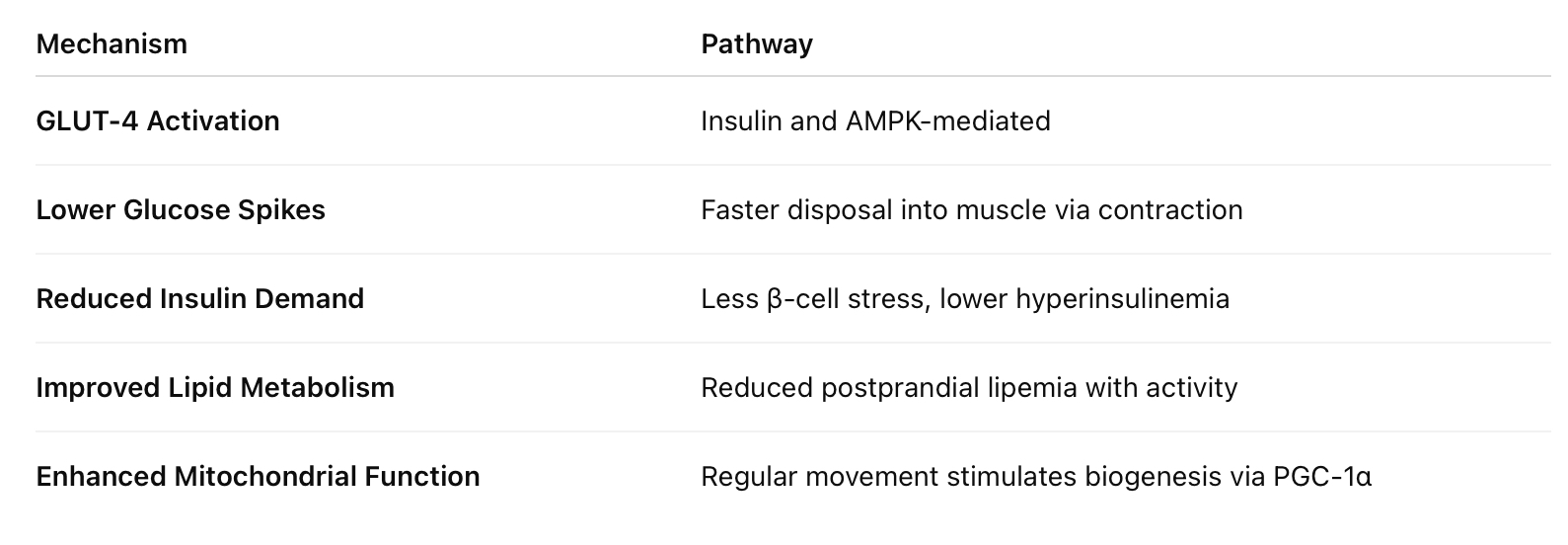
Mechanistic Summary
Final Thoughts
For trainers serious about long-term client outcomes, especially in the areas of fat loss, hormonal regulation, and disease prevention, postprandial walking is a non-negotiable tool. It’s low-barrier, evidence-backed, and physiologically potent.
Encouraging simple behaviors like walking after meals is not just “lifestyle advice”—it’s applied physiology that can transform a client’s metabolic trajectory.
References
-
DeFronzo, R. A., et al. (1988). Glucose intolerance and aging. Diabetes Care.
-
Holloszy, J. O. (2005). Exercise-induced increase in muscle insulin sensitivity. Journal of Applied Physiology.
-
Reynolds, A. N., et al. (2016). Walking breaks in prolonged sitting reduce postprandial glycemia in type 2 diabetes. Diabetologia.
-
Colberg, S. R., et al. (2016). Physical activity/exercise and diabetes. Diabetes Care.
-
Dempsey, P. C., et al. (2016). Interrupting prolonged sitting in type 2 diabetes. Diabetes Care.
